Page 1 GAO-19-74R Indian Health Service
441 G St. N.W.
Washington, DC 20548
December 10, 2018
The Honorable Ken Calvert
Chairman
The Honorable Betty McCollum
Ranking Member
Subcommittee on Interior, Environment, and Related Agencies
Committee on Appropriations
House of Representatives
Indian Health Service: Spending Levels and Characteristics of IHS and Three Other
Federal Health Care Programs
The Indian Health Service’s (IHS) mission is to provide health care services to American Indian
and Alaska Native (AI/AN) people who are members or descendants of federally recognized
tribes, consistent with federal law.
1
Congress has declared that it is federal policy, in fulfillment
of special trust responsibilities and legal obligations to Indians, to ensure the highest possible
health status for AI/AN people.
2
IHS, within the Department of Health and Human Services
(HHS), provides health care to approximately 1.6 million AI/AN people annually.
3
Advocates for AI/AN people have longstanding concerns about whether IHS has sufficient
funding to provide eligible individuals with all needed services, noting IHS's lower funding
relative to federal health programs for other populations (some of which include AI/AN people).
These other federal health programs include:
• The Veterans Health Administration (VHA), which is part of the Department of Veterans
Affairs (VA), which provides health care services for approximately 7 million veterans
and non-veterans;
4
• Medicare, which is overseen by HHS’s Centers for Medicare & Medicaid Services
(CMS), which pays for health care services for around 58 million persons aged 65 years
and older (among others); and
• Medicaid, which is jointly administered and financed by CMS and state governments,
which pays for health care services for about 74 million low-income individuals.
1
Federally recognized tribes have a government-to-government relationship with the United States and are eligible to
receive certain protections, services, and benefits by virtue of their status as Indian tribes. The Secretary of the
Interior publishes annually in the Federal Register a list of all tribal entities that the Secretary recognizes as Indian
tribes. As of July 23, 2018, there were 573 federally recognized tribes. See 83 Fed. Reg. 34863 (July 23, 2018).
2
25 U.S.C. § 1602.
3
The 1.6 million represents IHS’s user population, that is, those individuals who accessed a federally or tribally
operated facility at least once over the past 3 years. The user population is a subset of the total service population of
2.2 million, which is IHS’s estimate of the number of AI/AN users that could access its services.
4
There are approximately 20 million veterans in total, of which 9 million are enrolled in VHA, with approximately 7
million receiving care. The 7 million receiving care are defined by VHA as “unique patients”—uniquely identified
individuals treated by VHA, or whose treatment is paid for by VHA. The unique patient population includes about
700,000 non-veterans (e.g., family members, active duty military and reservists, employees receiving preventive
occupational immunizations).

Page 2 GAO-19-74R Indian Health Service
You asked us to compare IHS program characteristics, including spending levels, to those of
other federal health care programs. In this report, we present information on the spending levels
and program characteristics for IHS, VHA, Medicare, and Medicaid from 2013 through 2017.
To address this objective, we analyzed budget and program documents from the four programs
for the years 2013 through 2017, such as agency budgets and Congressional budget
justifications, and reports produced by the Medicare Trustees, the Medicaid and CHIP Payment
and Access Commission, and CMS. For each program, we examined total annual spending
levels and spending on a per capita basis.
5
To do so, for IHS and VHA, we analyzed total
obligations per fiscal year. For IHS, we then calculated the per capita spending amount by
dividing the total obligations by the number of individuals served.
6
For VHA, we used data that
are presented in VHA’s annual congressional budget submission on obligations per unique
patient. For Medicare and Medicaid, we analyzed expenditure data and relied on per capita
spending data publicly available in the sources noted above.
7
For each program, we refer to
these amounts as spending or spending on a per capita basis because they represent the
agencies’ use of funds for the provision of health care services. One inherent limitation to our
analysis is that the per capita spending amount for each program does not directly account for
spending for beneficiaries who are eligible for multiple federal programs. To supplement our
analysis, we interviewed knowledgeable agency officials, and, to obtain the perspective of tribal
communities, we also interviewed representatives from the National Indian Health Board and
attended a meeting of its National Tribal Budget Formulation Work Group, which makes
recommendations to IHS on tribal budget priorities.
We conducted this performance audit from December 2017 to November 2018 in accordance
with generally accepted government auditing standards. Those standards require that we plan
and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for
our findings and conclusions based on our audit objectives. We believe that the evidence
obtained provides a reasonable basis for our findings and conclusions based on our audit
objectives.
Background
IHS, VHA, Medicare, and Medicaid are diverse programs through which the federal government
is either a direct provider of health care services or pays for services as a public insurer.
Specifically, IHS and VHA provide health care services directly to eligible beneficiaries. Both
programs provide care through agency-administered hospitals and other health care facilities,
5
The programs have differing definitions of their user populations. Therefore, we use the term “individuals served” to
encompass IHS users (individuals receiving care from a federally or tribally operated facility within the last 3 years);
VHA unique patients (uniquely identified individuals treated by VHA or whose treatment is paid for by VHA); and
Medicare beneficiaries and Medicaid enrollees (individuals enrolled in either program in a specific year).
6
An “obligation” is a definite commitment that creates a legal liability of government for the payment of goods and
services ordered or received.
7
An “expenditure” is the actual spending of money or an outlay. We calculated Medicare and Medicaid spending
using expenditures because, in contrast to IHS and VHA, Medicare and Medicaid act as public insurers, reimbursing
for services provided. Because of the differences in the four programs’ operations and structures, the data we
obtained and report on the Medicare program are on a calendar year basis, and the data we obtained and report on
the IHS, VHA, and Medicaid programs are on a fiscal year basis. Medicaid per capita spending data for fiscal year
2017 were not publicly available at the time of this report, so for that year, we calculated spending using estimates
published by CMS’s Office of the Actuary.

Page 3 GAO-19-74R Indian Health Service
though IHS funds also pay for care provided by tribally operated facilities.
8
These programs also
contract with health care providers outside of agency-funded facilities to provide care for users
under certain circumstances—IHS’s Purchased/Referred Care (PRC) program and VHA’s
community care programs.
9
In contrast, Medicare and Medicaid act as public insurers for their
beneficiaries by reimbursing health care providers for covered health care services or
contracting with managed care plans to pay providers for services delivered to program
enrollees.
In addition, the programs’ administrative structures and eligibility requirements differ markedly,
and they are intended to serve different populations. (See table 1 for additional information on
the programs’ administrative structures and eligibility requirements.)
8
Under the Indian Self-Determination and Education Assistance Act, as amended, federally recognized Indian tribes
can enter into self-determination contracts or self-governance compacts with the Director of IHS to take over the
administration of IHS programs for Indians previously administered by IHS on their behalf. See generally 25 U.S.C.
§§ 5301-5423. In 2017, IHS transferred approximately 54 percent of its total budget to tribes and tribal organizations
to operate part or all of their own health care programs through self-determination contracts and self-governance
compacts. Under the Indian Health Care Improvement Act, IHS also awards contracts and grants to non-profit urban
Indian organizations that provide health care and referral services to urban Indians.
9
VHA also has the option to purchase care from community providers through a number of community care
programs, in circumstances when a health care service is not offered at a VA medical center or cannot be provided in
a timely manner.
Page 4 GAO-19-74R Indian Health Service
Table 1: Structure of and Eligibility for Four Federal Health Care Programs—Indian Health Service (IHS),
Veterans Health Administration (VHA), Medicare, and Medicaid
Program Item
IHS
VHA
Medicare
Medicaid
Administrativ
e structure
Direct provider.
• Within the
Department of
Health and Human
Services (HHS)
• Provides health
care services
through a network
of federally or
tribally operated
hospitals, clinics,
and health stations.
• Pays for health care
services
unavailable at these
facilities through its
Purchased/
Referred Care
program.
Direct provider.
• Within the
Department of
Veterans Affairs
• Provides services
through VHA-
administered
hospitals and other
health care
facilities.
• Pays for certain
care outside the
VHA health care
system through its
community care
programs.
Public insurer.
• Federal program
administered by the
Centers for
Medicare &
Medicaid Services
(CMS) within HHS.
• Pays health care
providers for
covered health care
services.
• Pays insurers for
health care services
delivered through
managed care
plans.
a
Public insurer.
• A joint federal-
state program—
administered by
the states, with
CMS oversight.
• Pays health care
providers for
covered health
care services.
• Pays insurers for
health care
services delivered
through managed
care plans.
a
Who is
eligible
• Members of a
federally
recognized Indian
tribe, or those who
meet certain other
requirements (e.g.,
actively
participating in tribal
affairs).
• Veterans, as
determined by a
number of service-
related factors,
such as the period
of active service,
discharge status,
and the presence
of service
connected
disabilities.
• Certain non-
veterans, such as
veterans’ spouses,
dependents, and
survivors.
• Persons aged 65
and older, certain
individuals with
disabilities, and
individuals with
certain conditions,
such as end-stage
renal disease.
• Certain low-
income
individuals, such
as pregnant
women, children,
the disabled, and
persons aged 65
and older.
b
Source: GAO analysis of program information. | GAO-19-74R
Notes: Individuals may be eligible for more than one program. For individuals eligible for IHS services, the IHS or tribally operated
facility may be reimbursed by VHA, Medicare, and Medicaid for care provided. When approving funding for services through
IHS’s Purchased/Referred Care program, IHS is the payer of last resort—that is, IHS will only pay for a service if the individual is
not eligible to have it covered by another program.
a
In managed care for Medicare and Medicaid, the federal government or states respectively contract with managed care plans to
provide a specific set of covered services to beneficiaries and pay them a set amount, typically per beneficiary per month, to provide
those services.
b
States are required to cover certain mandatory populations, such as low-income children and pregnant women, but have the option
to cover other populations, such as low-income, childless adults. As of June 2018, 33 states (including the District of Columbia)
have chosen to expand Medicaid to cover certain childless adults with incomes at or below 133 percent of the federal poverty level.
Page 5 GAO-19-74R Indian Health Service
IHS’s Spending Levels and Program Characteristics Vary from Those of VHA, Medicare,
and Medicaid
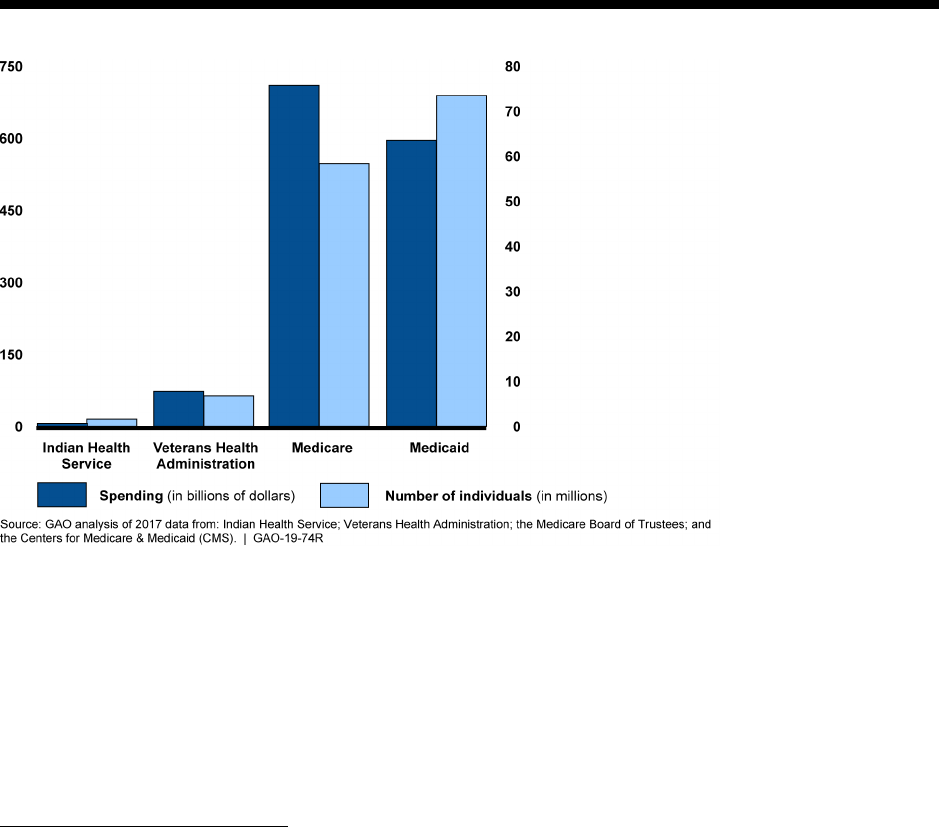
IHS is significantly smaller than VHA, Medicare, and Medicaid in terms of annual spending
levels and the number of individuals served. For example, in 2017, IHS’s total spending of $6.68
billion was less than 10 percent of VHA’s and about 1 percent of both Medicare’s and
Medicaid’s spending. In this same year, IHS served about 1.6 million individuals, about 25
percent of the number served by VHA and less than 3 percent of the number served by
Medicare and Medicaid (see fig. 1). Although spending and service levels varied over time,
these differences among the programs were also present in prior years. (See enclosures I
through IV for additional spending information about each of these four programs for 2013
through 2017.)
Figure 1: Spending Levels and Number of Individuals Served by Indian Health Service, Veterans Health
Administration, Medicare, and Medicaid, 2017
Notes: Spending levels for Indian Health Service (IHS) and Veterans Health Administration (VHA) are reported using total
obligations. IHS individuals served are those users who have accessed a federally or tribally operated facility at least once over the
past 3 years. For VHA, individuals served are “unique patients”—those uniquely identified individuals treated by VHA or whose
treatment is paid for by VHA. For Medicare and Medicaid, we report expenditures (including those by states for Medicaid), and
individuals served are beneficiaries and enrollees, respectively. Spending for Medicare represents total expenditures from the
Medicare trust funds and does not include beneficiary cost-sharing spending. The data for IHS, VHA, and Medicaid are for fiscal
year 2017, and the Medicare data are for calendar year 2017. Medicaid data are based on projections published by CMS’s Office of
the Actuary, as actual data were not yet available at the time of this report.
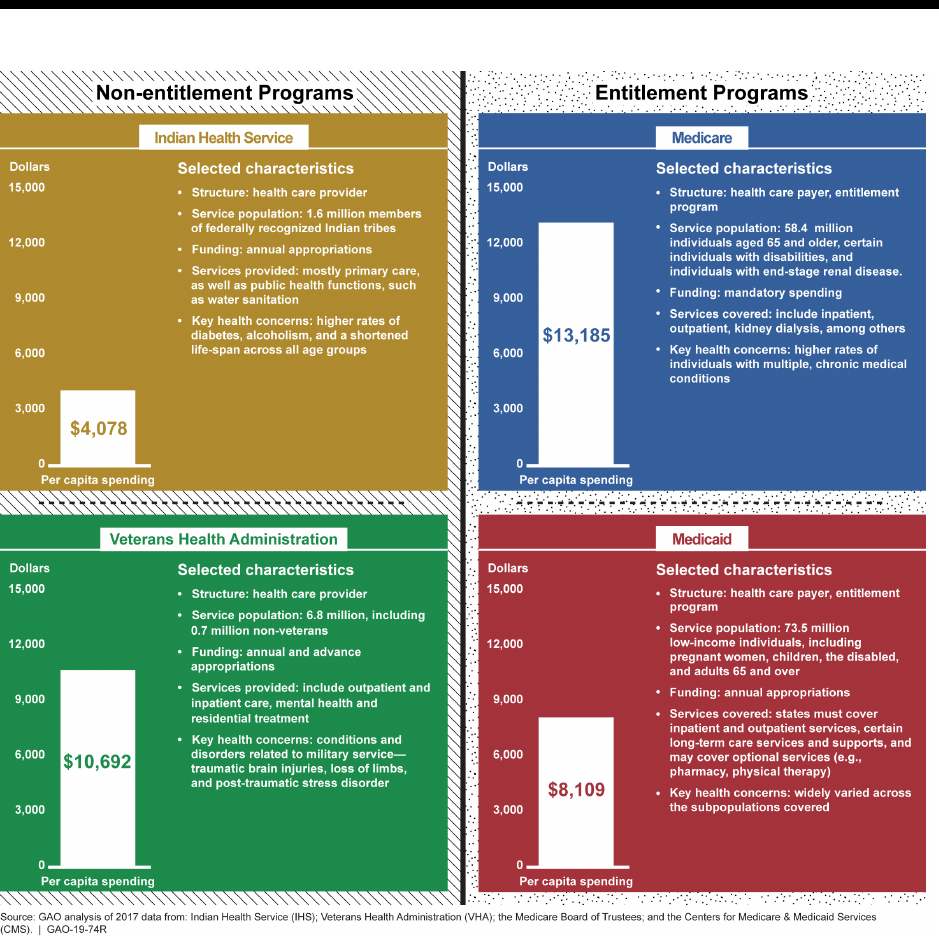
Our analysis showed that IHS’s per capita spending levels were likewise lower than those of the
other three programs.
10
For example, in 2017, IHS per capita spending was $4,078, as
compared to $8,109 for Medicaid, $10,692 for VHA, and $13,185 for Medicare.
11
In each of the
10
As discussed earlier, we calculated per capita spending as total obligations divided by the number of individuals
served for IHS and VHA, and total expenditures per individual beneficiary or enrollee for Medicare and Medicaid,
respectively. In the case of Medicaid, expenditures include spending by states.
11
We calculated IHS per capita spending using the agency’s 3-year reported user population for 2017—about 1.6
million. IHS also collects data on the number of users who accessed a facility each year—an average of about 1.3

Page 6 GAO-19-74R Indian Health Service
four programs, the per capita spending was relatively stable from 2013 through 2017, increasing
slightly for each program over the time period. While the per capita spending represents the
average amount of program spending per individual served, the amount does not necessarily
represent the total health spending for its beneficiaries since eligibility for one program does not
preclude eligibility for others. Therefore some individuals may receive or have services covered
through more than one program. For example, an AI/AN veteran may be eligible to receive care
from an IHS facility but may also be enrolled and eligible for care from VHA for service-
connected injuries, as well as enrolled in Medicare.
12
That individual may use the IHS facility for
primary health care and use VHA facilities or Medicare coverage for other specialty care. Total
health care spending for that individual would be captured across each of the three programs.
While examining per capita spending is one way to compare these programs, the vast
differences between IHS, VHA, Medicare, and Medicaid programs limit the applicability of such
comparisons. The programs differ in design and structure, funding, population needs, and the
services provided, for example. These fundamental differences limit the extent to which
comparisons of federal funding for each program can be used to make a determination about
the sufficiency of program funding:
• Program Design and Structure. Because IHS and VHA are direct health care providers, they
operate health care facilities and manage health care professionals as employees.
13
Medicare and Medicaid act as public insurers for their beneficiaries by reimbursing health
care providers for covered health care services. In addition, the four programs differ in how
funding is used for services beyond direct clinical care. For example, in addition to using
funding to partner with other federal agencies to build water sanitation systems, IHS
provides scholarships and loan repayment awards to recruit health professionals to serve in
areas with high provider vacancies. In the case of Medicare, a portion of the amount that it
reimburses certain facilities for care provided to patients is also intended to provide support
for physician graduate medical education at those facilities.
• Funding Mechanism. IHS and VHA funding is largely determined through the annual
appropriation process, with specific limits on the amounts that can be spent to deliver health
care services.
14
Thus, any increases in the number of people served in these two programs
absent increased funding could result in reductions in per capita spending. In contrast,
Medicare and Medicaid are entitlement programs—that is, the federal government is
required to pay for covered services for any person meeting eligibility criteria. In terms of
funding, Medicare is financed through payroll taxes, general revenues, and beneficiary
million, from fiscal years 2013 through 2017. Using this 1-year user population count, IHS’s per capita spending is
$5,173.
12
According to IHS data, in fiscal year 2017, approximately 75 percent of IHS individuals reported that they had at
least one other means of health care coverage. This estimate of the proportion of IHS users with additional coverage
is not an estimate of the extent to which they obtain services through additional coverage.
13
IHS and VHA also purchase some care from external providers.
14
Discretionary appropriations refer to those budgetary resources that are provided in appropriation acts, other than
those that fund mandatory programs. While IHS and VHA receive most of their funding from these appropriations,
they also receive mandatory spending authority for specific purposes. Mandatory spending refers to budget authority
that is provided in laws other than appropriation acts and includes entitlement authority. VA also receives advance
appropriation authority—an appropriation of new budget authority that becomes available one or more fiscal years
after the fiscal year for which the appropriation providing it is enacted. See 38 U.S.C § 117. Legislation has been
introduced in the House to provide IHS with advance appropriation authority, and we recently reported on the issue.
See GAO, Indian Health Service: Considerations Related to Providing Advance Appropriation Authority, GAO-18-652
(Washington, D.C.: Sept. 13, 2018).

Page 7 GAO-19-74R Indian Health Service
contributions.
15
Medicaid is financed through a combination of federal and state funding.
16
As entitlement programs, Medicare and Medicaid have no annual spending caps. Instead,
spending for Medicare and Medicaid is controlled by Congress through a modification of
benefits or changes to the way providers are paid.
• Service Availability. While each of the programs can pay for a wide variety of services, there
are differences in the actual availability of certain services. Medicare and Medicaid pay for
primary and specialty services in a variety of hospital and other settings in all parts of the
country. In contrast, IHS and VHA facilities vary in the extent to which services are available.
For example, VHA medical centers offer a variety of inpatient and outpatient services,
ranging from routine examinations to complex surgical procedures. VHA’s system also
includes facilities such as community-based outpatient clinics. In the case of IHS, most of its
facilities are smaller and may offer mostly primary and emergency care services. These IHS
facilities also tend to be located primarily in rural areas where patients and providers must
travel long distances, and where other health care providers are not available.
17
While IHS is
able to use its PRC program to pay for care not available at these facilities, the agency has
reported that PRC funds are not sufficient to pay for all necessary care and, therefore,
generally pay for only the highest priority costs, such as emergency care and transportation
to that care. (See enclosure V for more information about the PRC program.)
• Population Needs and Services Provided. The four programs serve populations with
different health needs and issues and therefore provide or pay for a wide variety of services
with varying costs. For example, while IHS has a younger population overall, its users have
higher rates of diabetes, alcoholism, and accidental deaths than the general population.
Medicare enrollees, on the other hand, tend to be older and need more in-patient care—in
addition, a subset are eligible for Medicare coverage because they have end-stage renal
disease and require ongoing kidney dialysis, a long-term and costly treatment. In each of
these programs, the needs of the population impacts the services needed, and the services
provided will impact the per capita costs.
(See fig. 2 for 2017 per capita spending levels and selected program characteristics for each of
the four federal health programs.)
15
Funds from beneficiary contributions are deposited into the Medicare trust funds that are overseen by the Medicare
Board of Trustees.
16
State Medicaid expenditures are matched by the federal government on the basis of a statutory formula. Medicaid is
considered an appropriated entitlement because, although it is an entitlement program, its funding is provided in
annual appropriation acts. CMS estimates Medicaid expenditures for the fiscal year and Congress appropriates that
amount. For the final quarter of the fiscal year, Congress also appropriates such sums as may be necessary for any
unanticipated costs.
17
We recently reported that IHS officials told us that the agency provides services almost exclusively in locations
designated by HHS’s Health Resources and Services Administration as Health Professional Shortage Areas, or
extreme shortage areas, meaning they lack sufficient number of primary care physicians. See GAO, Indian Health
Service: Agency Faces Ongoing Challenges Filling Provider Vacancies, GAO-18-580 (Washington, D.C.: Aug. 15,
2018).
Page 8 GAO-19-74R Indian Health Service
Figure 2: 2017 Per Capita Spending Levels and Selected Program Characteristics for Four Federal Health
Programs: Indian Health Service, Veterans Health Administration, Medicaid, and Medicare
Notes: Some individuals may receive or have services covered through more than one program; however, the reported per capita
spending amounts do not account for spending across multiple programs. While IHS and VHA receive most of their funding from
annual appropriations, they also received mandatory amounts for specific purposes. For IHS we calculated per capita spending as
total obligations divided by the number of individuals served. IHS defines individuals served as those who have accessed a federally
or tribally operated facility at least once over the past 3 years. For VHA, the per capita spending represents obligations per unique
patient (uniquely identified individuals treated by VHA or whose treatment is paid for by VHA). For Medicare and Medicaid, we report
on expenditures (including those by states for Medicaid) by the number of individuals served. Spending for Medicare represents
total expenditures from the Medicare trust funds and does not include beneficiary cost-sharing spending. The data for IHS, VHA,
and Medicaid are for fiscal year 2017, and the Medicare data are for calendar year 2017. The Medicaid data are based on estimates
published by CMS’s Office of the Actuary, as actual data were not yet available at the time of this report.
Page 9 GAO-19-74R Indian Health Service
Agency Comments
We provided a draft of this report to HHS and VA. Both departments provided us with technical
comments, which we incorporated as appropriate.
_ _ _ _ _
We are sending copies of this report to the Secretary of Health and Human Services, Secretary
of Veterans Affairs, and other interested parties. In addition, the report is available at no charge
on the GAO website at http://www.gao.gov.
If you or your staffs have any questions about this information, please contact me at (202) 512-
7114 or [email protected]. Contact points for our Offices of Congressional Relations and Public
Affairs may be found on the last page of this report. GAO staff who made key contributions to
this report were William D. Hadley, Assistant Director; Kristeen McLain, Analyst-in-Charge;
Manuel Buentello; and Keith Haddock. Also contributing were Muriel Brown, Jackie Hamilton,
Laurie Pachter, and Vikki Porter.
Jessica Farb
Director, Health Care
Enclosures – 5
Page 10 GAO-19-74R Indian Health Service
Enclosure I: Indian Health Service
Enclosure I
Indian Health Service
Annual Spending and Numbers Served
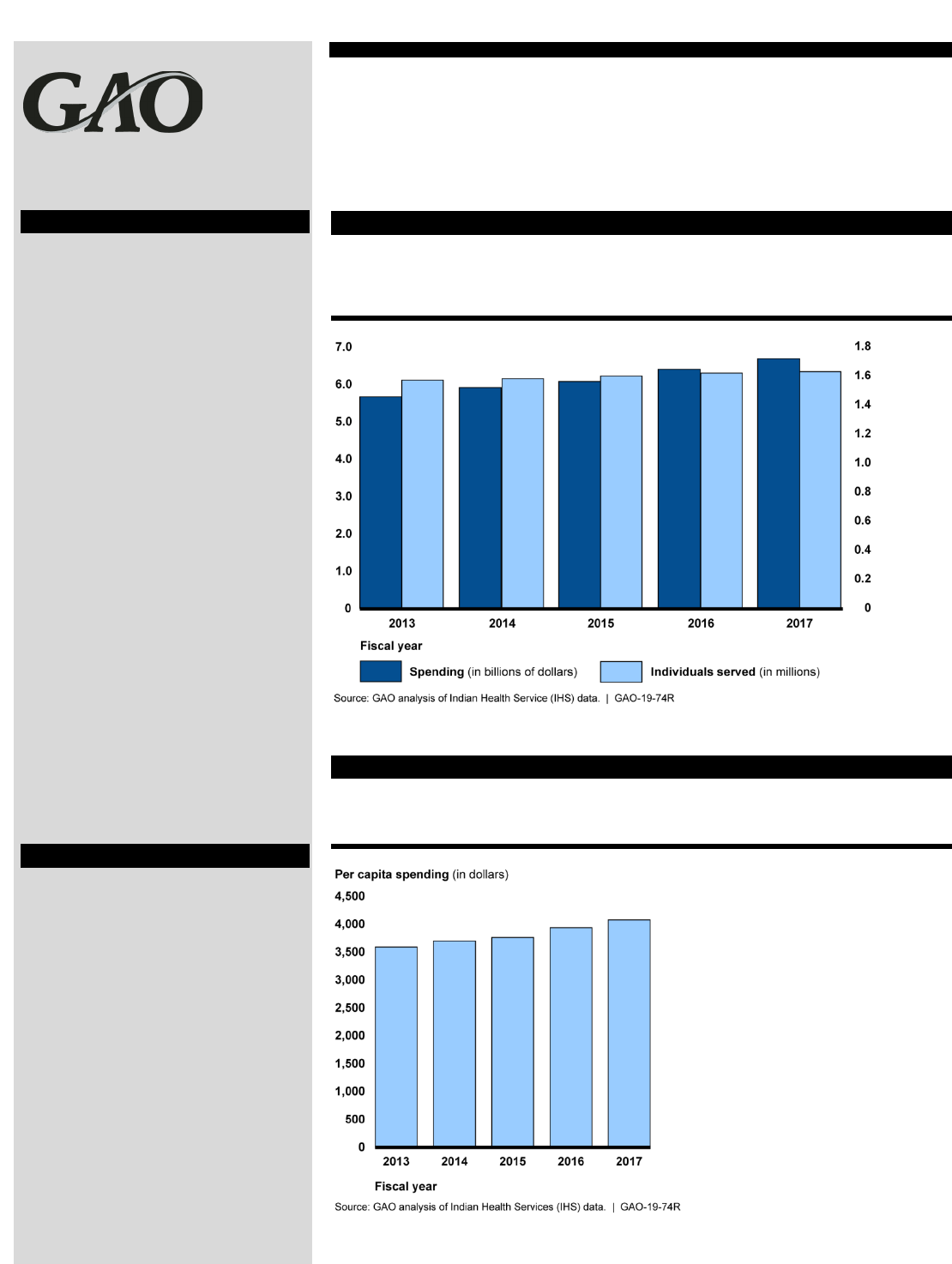
According to our analysis, from fiscal years 2013 through 2017, IHS’s
annual spending increased from $5.66 billion to $6.68 billion (18 percent),
while the annual population served remained around 1.6 million.
Figure 3: IHS Spending and Number of Individuals Served, Fiscal Years 2013-2017
Notes: Spending is in total obligations. Individuals served are referred to as “users” by IHS, and are
defined as a person who has accessed IHS at least once over the past 3 years.
Per Capita Spending
Over the past five fiscal years, IHS’s per capita spending increased from
$3,591 to $4,078 (14 percent).
Figure 4: IHS Per Capita Spending, Fiscal Years 2013-2017
Notes: To calculate per capita spending, we analyzed IHS’s total obligations. We then divided the
spending amount by the number of individuals served, which are defined by IHS as a person who has
accessed services at least once over the past 3 years.
Program Overview
The Indian Health Service (IHS)
was established within the Public
Health Service in 1955 to provide
health services to American Indian
and Alaska Native (AI/AN) people.
IHS provides services directly
through a network of 26 hospitals,
53 health centers, and 30 health
stations in 37 U.S. states, primarily
in rural areas on or near
reservations. IHS also awards
contracts and grants to non-profit
urban Indian organizations that
provide health care and referral
services to urban Indians. IHS also
funds services provided at tribally
operated facilities. In fiscal year
2017, about 54 percent of IHS
funds went to tribal organizations.
In certain circumstances, IHS pays
for services provided by external
providers through its
Purchased/Referred Care program.
In addition to the provision of
health care, IHS performs several
public health functions, including
public health nursing and water
sanitation facility construction.
How Funded
IHS is largely funded through
discretionary appropriations, but
also receives some funding
through reimbursements from other
federal programs such as
Medicaid, Medicare, and the
Veterans Health Administration, as
well as private insurance. IHS also
receives mandatory spending
authority (around $150 million
annually) to support Special
Diabetes Programs for Indians.
Page 11 GAO-19-74R Indian Health Service
Enclosure I: Indian Health Service
Enclosure I
Indian Health Service (con’t.)
User Characteristics
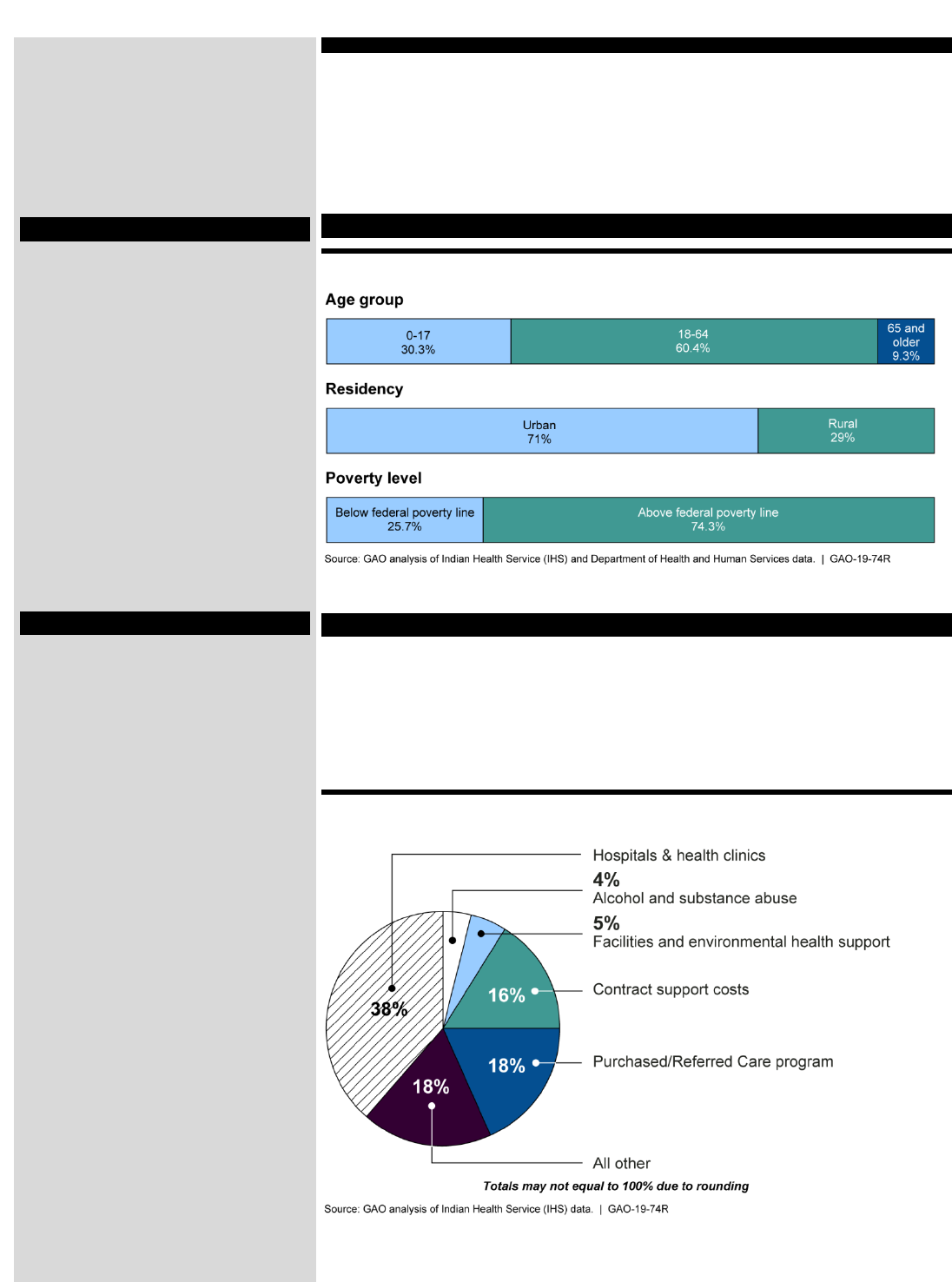
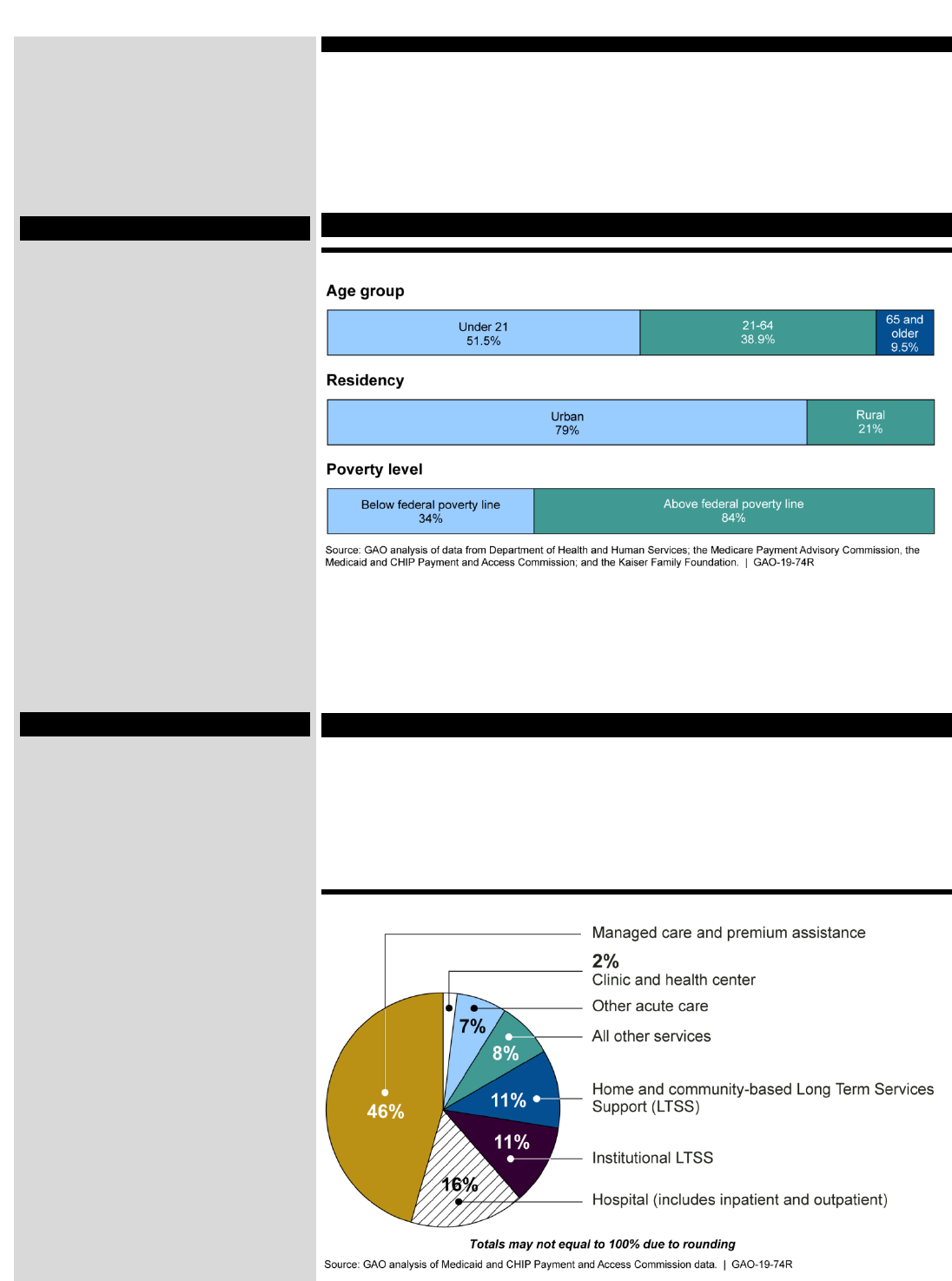
Figure 5: Selected Characteristics of IHS Users
Notes: Age group data are fiscal year 2017, residency data are calendar year 2010, and poverty data
are calendar year 2000.
Services
According to our analysis, in fiscal year 2017, just over one-third of IHS's
budget was allocated to hospitals and health clinic services. IHS also
funded several service categories outside direct health care. For
example, 16 percent of funds were allocated to contract support costs—
supporting required activities that ensure tribes’ compliance with their
self-governance agreements.
Figure 6: IHS Services Provided by Percentage of Funding, Fiscal Year 2017
Notes: Funding for services is measured in budget authority. IHS’s Purchased/Referred Care
program pays for care when those services are not available at federally operated or tribally operated
IHS facilities. Contract support costs cover required activities to ensure compliance with their self-
determination contracts and self-governance compacts.
Eligibility
IHS users generally must be a
member or descendant of one of
the 573 currently federally
recognized Indian tribes belonging
to the Indian community, as
evidenced by such factors as
membership, residence on tax-
exempt land, active participation in
tribal affairs, or other relevant
factors. IHS services are provided
free to eligible IHS users and there
are no cost-sharing requirements.
Health Issues
According to IHS, AI/AN people die
at higher rates in many categories,
including chronic liver disease and
cirrhosis, diabetes mellitus,
unintentional injuries, assault or
homicide, intentional self-harm or
suicide, and chronic lower
respiratory diseases.
IHS provides a number of health
services that target common health
conditions among beneficiaries,
such as diabetes prevention and
treatment, and behavioral health
services including suicide
prevention and methamphetamine
treatment.
Page 12 GAO-19-74R Indian Health Service
Enclosure II: Veterans Health Administration
Enclosure II
Veterans Health Administration
Annual Spending and Numbers Served
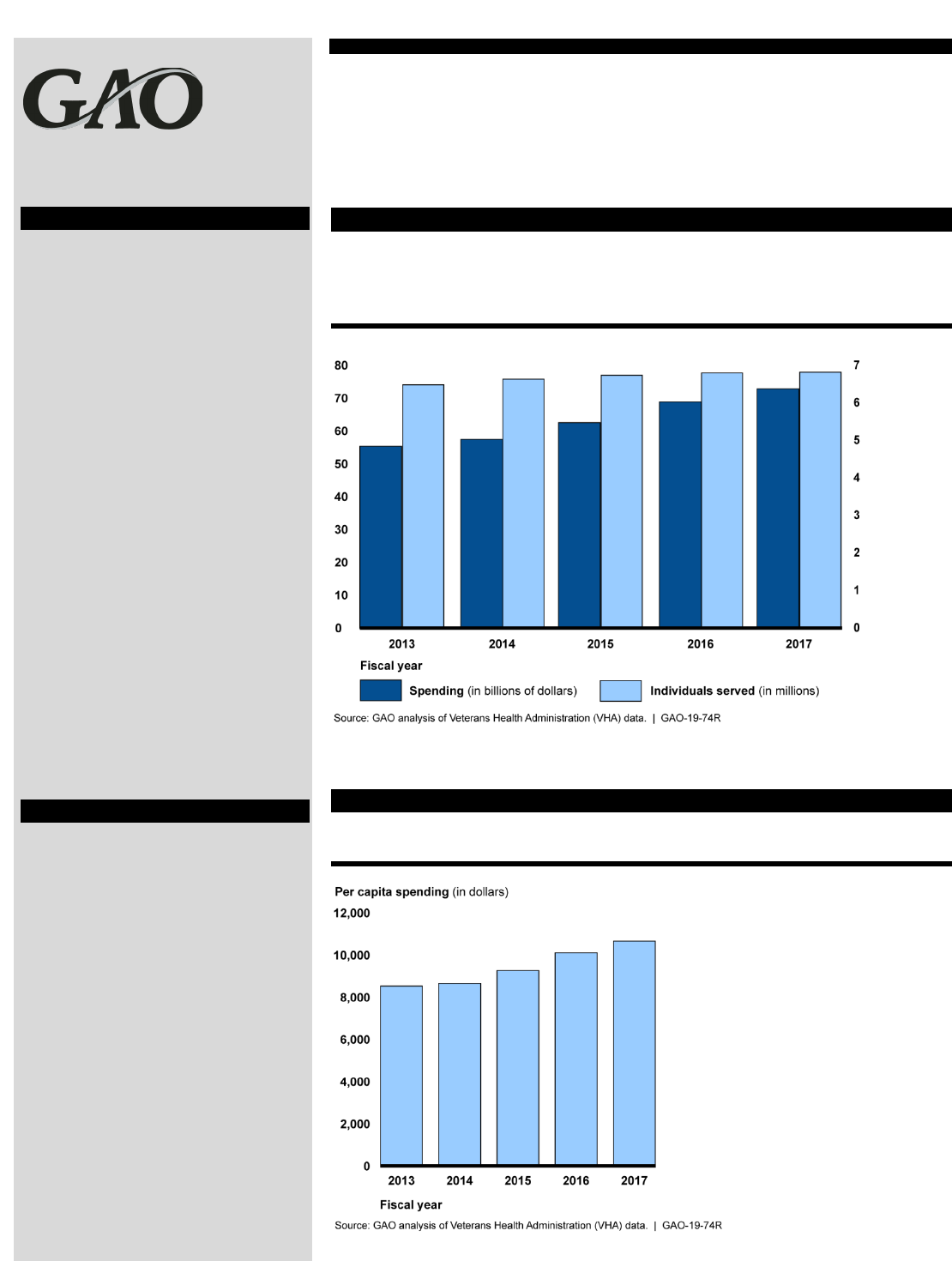
According to our analysis, from fiscal years 2013 through 2017, VHA’s
annual spending level increased from $55 to $73 billion (32 percent),
while the number of individuals served increased from 6.5 million to 6.8
million (5 percent).
Figure 7: VHA Spending and Number of Individuals Served, Fiscal Years 2013-2017
Note: Spending represents total obligations per fiscal year. Individuals served are “unique patients”
and represent uniquely identified individuals treated by VHA or whose treatment is paid for by VHA
expenditures.
Per Capita Spending
Over the past five fiscal years, per capita spending for VHA increased
from $8,551 to $10,692 (25 percent).
Figure 8: VHA Per Capita Spending, Fiscal Years 2013-2017
Note: Spending per capita represents total obligations per unique patient—uniquely identified
individuals treated by VHA or whose treatment is paid for by VHA expenditures.
Program Overview
The Veterans Health
Administration (VHA), part of the
Department of Veterans Affairs
(VA), established a network of
facilities to provide health care to
veterans, in particular to help them
recover from illnesses and injuries
sustained in service to the country.
In addition to providing services
through agency-administered
facilities—hospitals, outpatient
clinics, and nursing homes—VHA
can also pay for services outside
its health care system for eligible
veterans through its community
care programs when care is not
readily available at its medical
facilities.
How Funded
The VHA program is largely funded
through discretionary
appropriations. VA (which oversees
VHA) also receives advance
appropriations—an appropriation of
new budget authority that becomes
available one or more fiscal years
after the fiscal year for which the
appropriation providing it is
enacted—for specified medical
care accounts. In addition, VHA
can be reimbursed by private
insurance for services that are not
service-connected. While VHA
users do not pay premiums, some
users may have to pay copayments
for certain medical services.
Page 13 GAO-19-74R Indian Health Service
Enclosure II: Veterans Health Administration
Enclosure II
Veterans Health Administration (con’t.)
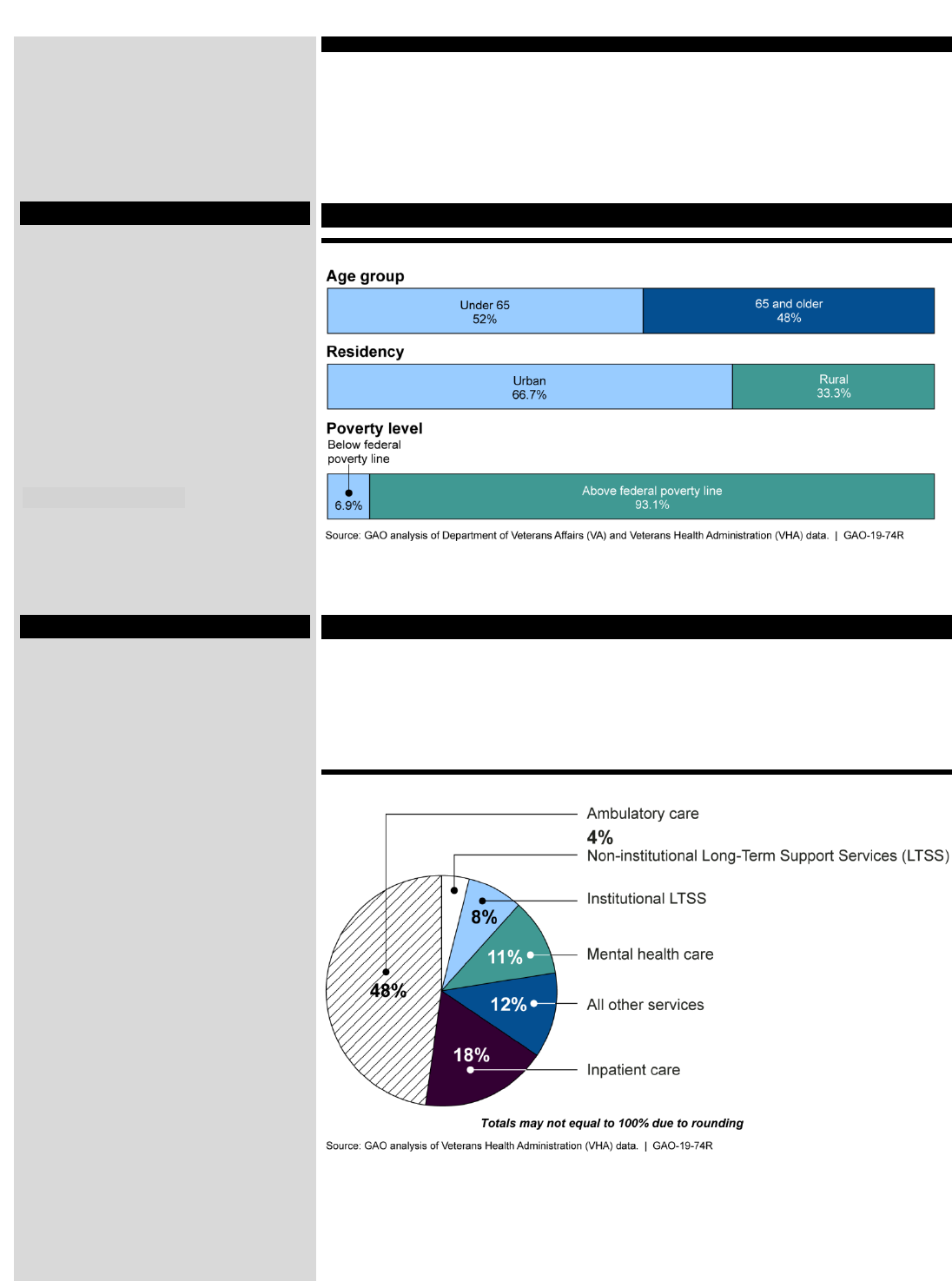
User Characteristics
Figure 9: Selected Characteristics of the Veteran Population
Note: The age group and residency data represent VHA’s unique patient populations for fiscal year
2017 and fiscal year 2015, respectively. The poverty data represent the total veterans population, and
are based on a 3-year period estimate, 2010 through 2012.
Services
VHA’s health care system provides enrolled veterans with a full range of
services including primary care, mental health, inpatient care, and
residential treatment. In fiscal year 2017, close to half of the expenditures
for services provided by VHA were for ambulatory (outpatient) care,
according to our analysis.
Figure 10: VHA Services Provided by Expenditures, Fiscal Year 2017
Eligibilty
Eligibility for services provided
through the VHA is based on
several factors, including the
veteran’s period of active service,
discharge status, and the presence
of service connected disabilities. In
addition, VHA categorizes eligible
veterans into eight priority groups
that determine the type of services
the veteran can access, and that
have implications for cost-sharing.
Eligibility for VHA’s community
care programs vary.
Health Issues
VHA focuses on conditions and
disorders related to military service
and war, including traumatic brain
injuries, post-traumatic stress
disorder, mental health issues,
such as suicide prevention, and
loss of limbs.
Page 14 GAO-19-74R Indian Health Service
Enclosure III: Medicare
Enclosure III
Medicare
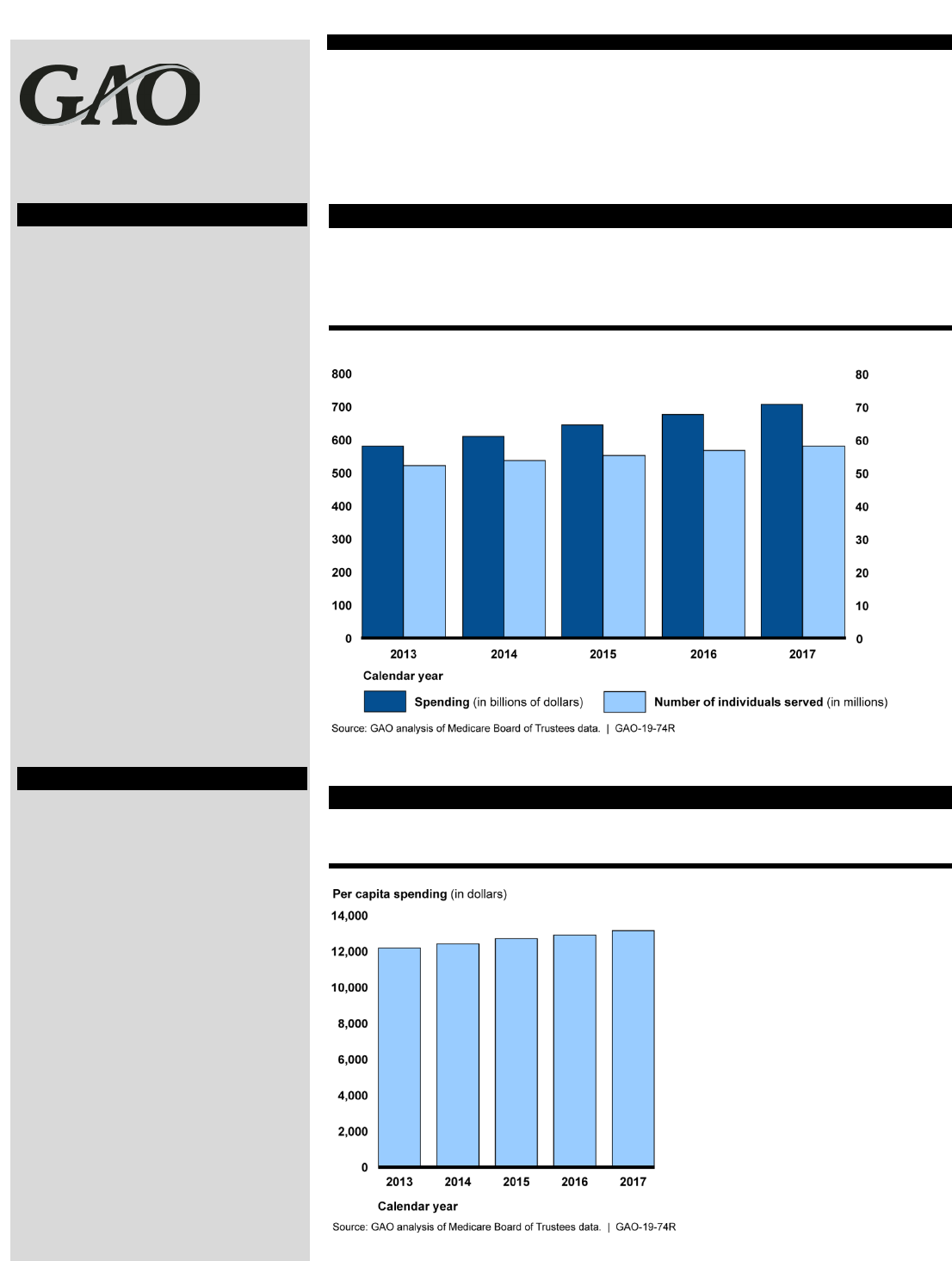
Annual Spending and Numbers Served
According to our analysis, from calendar years 2013 through 2017
Medicare spending increased by 22 percent, from $583 billion to $710
billion. During that same period, the number of individuals served grew
about half as much, by 10 percent.
Figure 11: Medicare Spending and Number of Individuals Served, Calendar Years
2013-2017
Note: Spending represents total expenditures from the Medicare trust funds and does not include
beneficiary cost-sharing spending. Individuals served are Medicare beneficiaries.
Per Capita Spending
Over the past five calendar years, Medicare per capita spending
increased from $12,218 to $13,185 (8 percent).
Figure 12: Medicare Per Capita Spending, Calendar Years 2013-2017
Note: Per capita spending represents average expenditures from the Medicare trust funds, and does
not include beneficiary cost-sharing spending.
Program Overview
The Medicare program, established
under Title XVIII of the Social
Security Act in 1965, pays for
health services for individuals 65
and older and individuals with
certain disabilities and conditions.
The program is administered by the
Centers for Medicare & Medicaid
Services (CMS) within the U.S.
Department of Health and Human
Services. Medicare consists of four
distinct parts (A through D). Part A
covers inpatient hospital services,
skilled nursing care, hospice care,
and some home health services.
Part B covers physician services,
outpatient services, and some
home health and preventive
services. Part C (Medicare
Advantage) is a private plan option
for beneficiaries, and covers all
Parts A and B services except
hospice. Lastly, Part D covers
outpatient prescription drug
benefits.
How Funded
Medicare is funded through payroll
taxes paid by employees and
employers, general revenues, and
interest on the Medicare trust
funds. Medicare is also funded
through premiums paid by
beneficiaries. Beneficiaries also are
responsible for cost sharing—
deductibles and co-payments—for
covered services. Medicare is an
entitlement program and required
to pay for all covered services
provided to eligible persons, so
long as specific criteria are met.
Thus, spending under the program
(except for a portion of
administrative costs) is considered
mandatory and is not subject to
spending caps in appropriation
acts.
Page 15 GAO-19-74R Indian Health Service
Enclosure III: Medicare
Enclosure III
Medicare (con’t.)
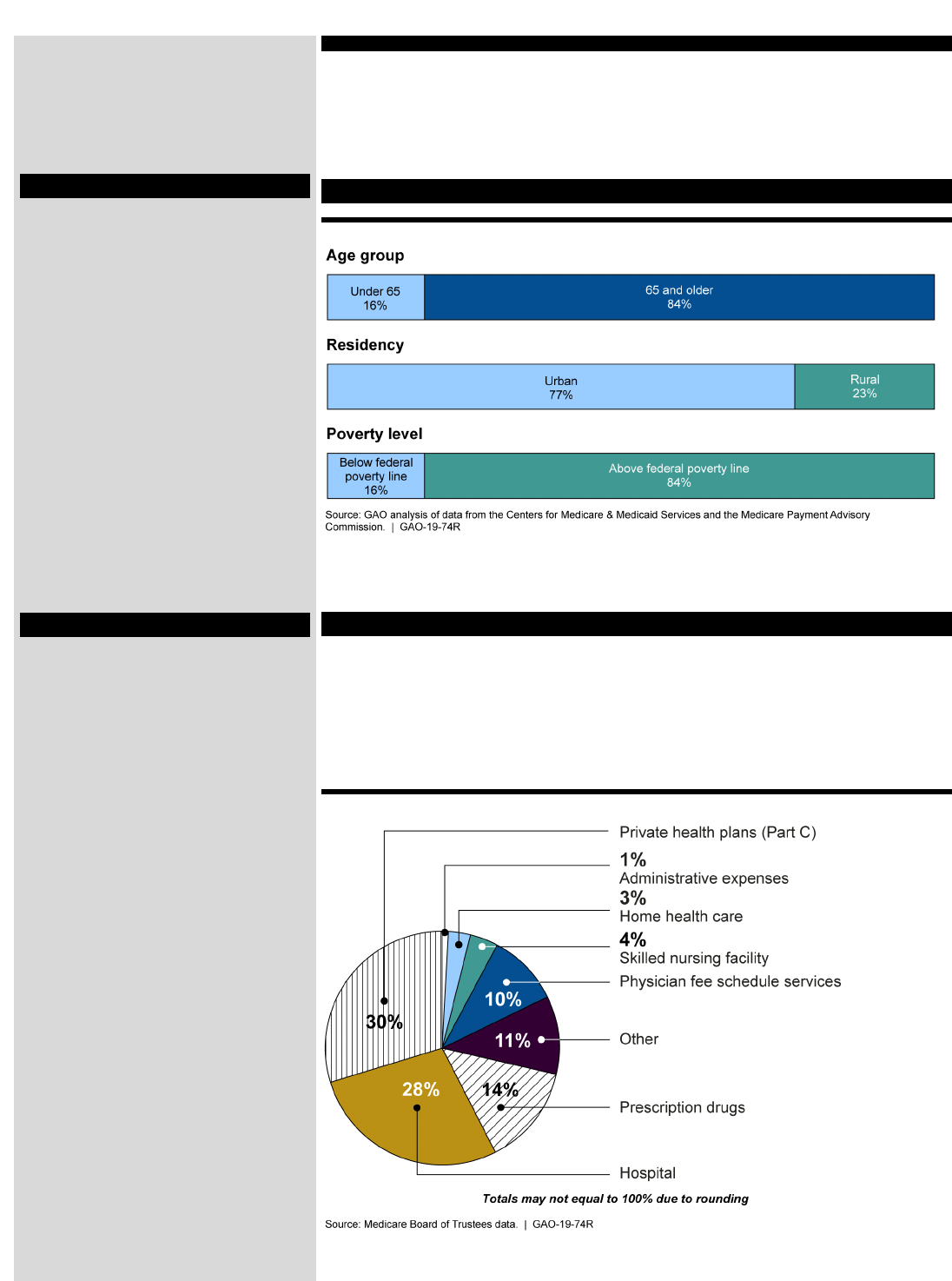
User Characteristics
Figure 13: Selected Characteristics of Medicare Beneficiaries
Notes: The age group and residency data represent the Medicare beneficiary population for calendar
year 2015 and 2013, respectively. The poverty data represent calendar year 2013.
Services
The Medicare program covers a wide variety of services, including
inpatient and outpatient care, some home health and preventive services,
and prescription drug benefits. In calendar year 2017, our analysis
showed that 30 percent of Medicare spending was for Part C (Medicare
Advantage), followed by hospital care (28 percent) and prescription drugs
(14 percent).
Figure 14: Medicare Services by Percentage of Expenditures, Calendar Year 2017
Note: These expenditures exclude cost-sharing spending by Medicare beneficiaries.
Eligibility
Generally, individuals are eligible
for Medicare if they or their spouse
worked for at least 40 quarters in
Medicare-covered employment,
are 65 years old, and are a citizen
or permanent resident of the
United States. Younger individuals
who have been eligible for Social
Security benefits for 24 months are
also eligible, as are those who
have end-stage renal disease
(permanent kidney failure requiring
dialysis or transplant), or have
amyotrophic lateral sclerosis (ALS,
Lou Gehrig’s disease).
Health Issues
Medicare serves approximately
one in six Americans and virtually
all of the population aged 65 and
older. Leading causes of death
among people 65 and over have
remained the same over the past
few decades, with heart disease
and cancer remaining at the top
followed by chronic respiratory
issues and stroke. In addition, the
Medicare population has high rates
of individuals with multiple, chronic
medical conditions.
Page 16 GAO-19-74R Indian Health Service
Enclosure IV: Medicaid
Enclosure IV
Medica
id
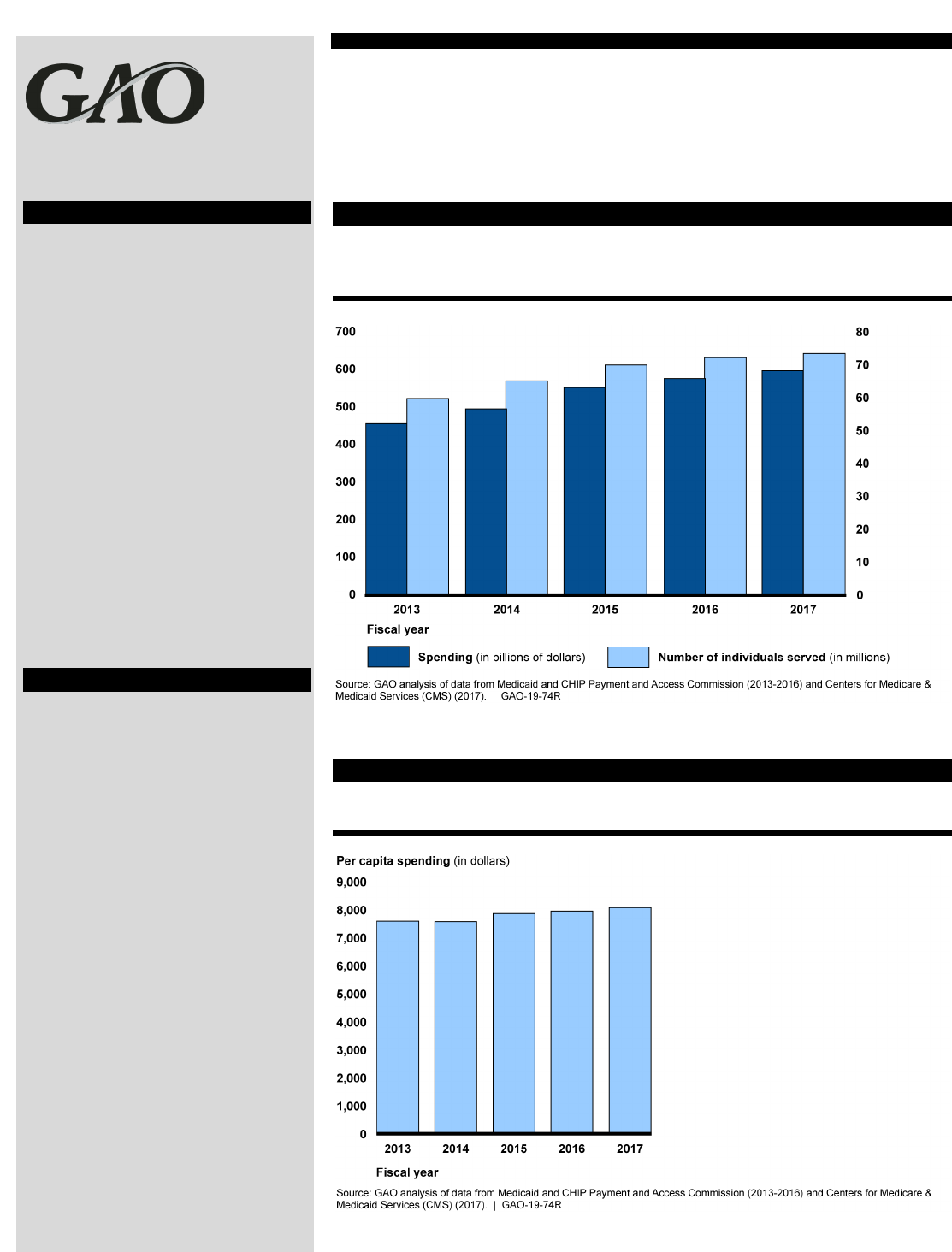
Annual Spending and Numbers Served
According to our analysis, from fiscal years 2013 through 2017, Medicaid
spending increased from $456 billion to $596 billion (31 percent), while
enrollment grew from 59.8 million to 73.5 million (23 percent).
Figure 15: Medicaid Spending and Number of Enrollees, Fiscal Years 2013-2017
Notes: Spending consists of federal and state Medicaid expenditures for benefits and administration,
excluding the Vaccines for Children program. Enrollment counts are full-year equivalents. Data for
fiscal year 2017 are based on CMS estimates and were the most recent available.
Per Capita Spending
Over the past five fiscal years, Medicaid spending per capita increased
from $7,615 in to $8,109 (6 percent).
Figure 16: Medicaid Per Capita Spending, Fiscal Years 2013-2017
Notes: Spending consists of federal and state Medicaid expenditures for benefits and administration,
excluding the Vaccines for Children program. Enrollment counts are full-year equivalents. Data for
fiscal year 2017 are based on CMS estimates and were the most recent available.
Program Overview
Medicaid—a joint federal-state
health financing program for low-
income and medically needy
individuals—was authorized by
Title XIX of the Social Security Act
in 1965. The Centers for Medicare
& Medicaid Services (CMS)
oversees states’ administration of
Medicaid. States are allowed
flexibility to design and implement
their programs within broad federal
parameters, resulting in variation in
eligibility and services covered
across the states.
How Funded
The federal government and states
share in the financing of Medicaid
expenditures, with the federal
government matching most state
expenditures for services on the
basis of a statutory formula, known
as the federal medical assistance
percentage. The federal share of
Medicaid expenditures typically
ranges from 50 to 83 percent.
Funding for Medicaid is provided in
annual appropriations acts, but is
not subject to specific dollar limits.
Page 17 GAO-19-74R Indian Health Service
Enclosure IV: Medicaid
Enclosure IV
Medicaid (con’t.)
User Characteristics
Figure 17: Selected Characteristics of Medicaid Enrollees
Notes: The age group and residency data represent Medicaid enrollee population for fiscal year 2013
and calendar year 2013, respectfully. The residency data exclude nondisabled enrollees under age
65, and those ages 65 and older who did not have Medicare coverage. The poverty data represent
Kaiser Family Foundation estimates based on Census Bureau data, 2014-2017.
Services
Medicaid provides a wide variety of services in order to provide care for
its diverse enrollee population, that includes children, adults, the disabled,
and the elderly. In fiscal year 2016, spending on managed care and
premium assistance made up almost 50 percent of total Medicaid
expenditures, followed by hospital services (both inpatient and outpatient)
at 16 percent.
Figure 18: Medicaid Services, by Expenditures, Fiscal Year 2016
Eligibility
Eligibility for Medicaid varies
across states. Federal law requires
states to cover certain populations
and gives them the flexibility to
cover others. Mandatory
populations include low-income
children and families, pregnant
women, and aged, blind and
disabled individuals. States may
also cover other populations. For
example, under the Patient
Protection and Affordable Care
Act, states may expand their
Medicaid programs to cover
childless, non-elderly low-income
adults. Medicaid enrollment is
therefore expected to grow by as
many as 13.2 million newly eligible
adults by 2025.
Health Issues
Health concerns vary considerably
among the different Medicaid
populations. For example, the
health concerns for children
enrolled in Medicaid center on
primary and preventive care, with a
small proportion requiring
medically complex care. In
contrast, Medicaid beneficiaries
who qualify on the basis of a
disability may have conditions such
as traumatic brain injuries,
intellectual or developmental
disabilities (such as cerebral palsy)
or serious behavioral disorders or
mental illness (such as
schizophrenia), all of which require
longer-term and high-cost care.

Page 18 GAO-19-74R Indian Health Service
Enclosure V: Indian Health Service’s Purchased/Referred Care Program
When an Indian Health Service (IHS) user needs health care services that are not available
from providers at a federal or tribal facility, the IHS Purchased/Referred Care (PRC) program
pays for services from external providers. Eligibility requirements for the PRC program are more
restrictive than for services provided directly through a facility, and all PRC requests are
categorized according to a medical priority system to help ensure that the program funds
services for the most serious medical conditions.
18
Therefore, not all requests for PRC program
funding are approved.
We obtained and analyzed data from IHS on the PRC program for fiscal years 2013 through
2017, including the expenditures and type of services paid through federally administered
facilities. We also analyzed the number of requests for payment that were not approved. These
data represent federally operated facilities—which in fiscal year 2017 represented about 46
percent of all IHS expenditures—and some tribally operated facilities, which are encouraged,
but not required, to report such data. We performed data reliability checks, such as checks for
internal consistency on total services and comparison of service expenditures to the PRC
program budgets, and determined the PRC program data were sufficiently reliable for our
purposes.
PRC Program Spending and Services
The PRC program is funded through the annual appropriations process, and available funds are
distributed to federally and tribally operated facilities based on a formula.
19
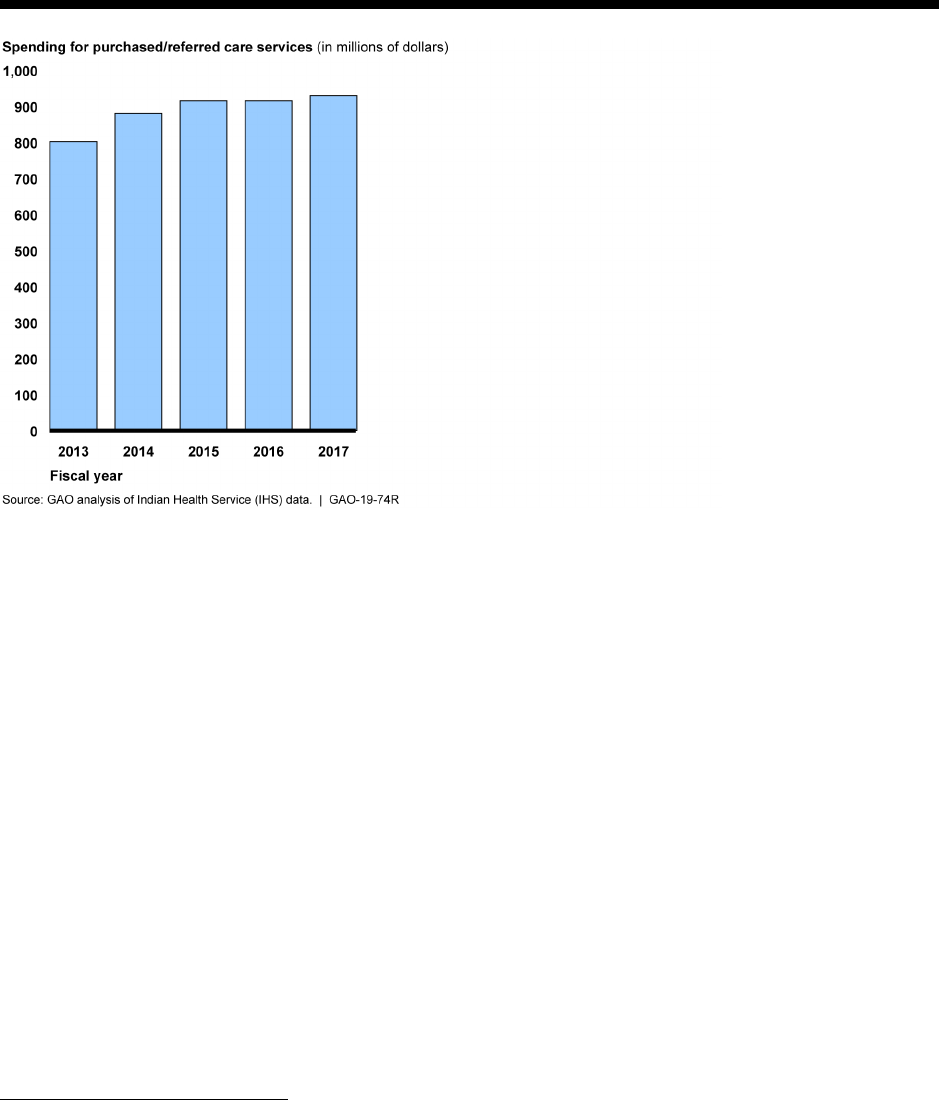
Spending for the
PRC program grew from $801 million in fiscal year 2013 to $929 million in fiscal year 2017, an
increase of 16 percent. (See fig. 19.)
18
IHS’s medical priority levels are: (1) Emergent or Acutely Urgent Care Services; (2) Preventive Care Services; (3)
Primary and Secondary Care Services; (4) Chronic Tertiary Care Services; and (5) Excluded Services. IHS users
who receive services paid through the PRC program must live within a specific geographic area for each facility;
these areas are smaller than other IHS service areas. Furthermore, the IHS user must also demonstrate that other
health care resources are not available to pay for the needed services.
19
See GAO, Indian Health Service: Action Needed to Ensure Equitable Allocation of the Resources for the Contract
Health Service Program GAO-12-446 (Washington, D.C.: Jun. 15, 2012). “Contract Health Service Program” is the
former name of the PRC program. In addition to receiving federal funding through IHS, the tribes may provide
supplemental funds to the PRC programs they administer.
Page 19 GAO-19-74R Indian Health Service
Figure 19: Indian Health Service Purchased/Referred Care Spending, Fiscal Years 2013-2017
Facilities can use PRC program funds to pay for a wide variety of services not available in the
facility. Between fiscal years 2013 and 2017 PRC program expenditures associated with
inpatient services ranged from 36 to 45 percent.
20
During that same period, outpatient services
expenditures ranged from 43 to 51 percent and patient transportation expenditures were 10 to
11 percent of expenditures.
21
Not All Requests for PRC Services Are Funded
Facilities do not approve all requests for services made through the PRC program. Requests
may be denied because the user did not meet PRC eligibility requirements, or because the
services were not within the medical priority for which funding is available. A facility may also
defer requests to pay for services until funding becomes available.
22
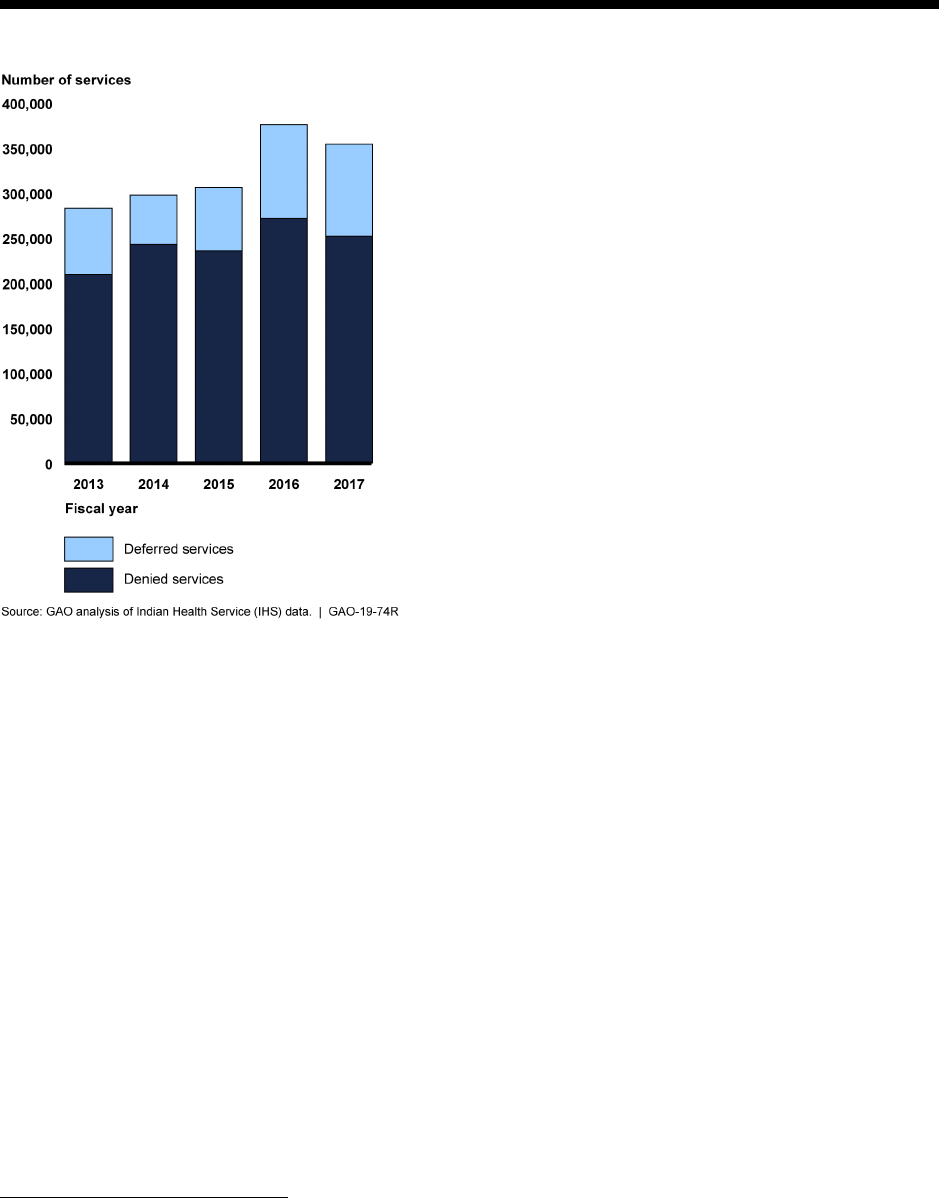
The number of deferred and denied services in federally and tribally operated facilities grew
from 283,020 services overall in fiscal year 2013 to 354,446 services in fiscal year 2017, an
increase of about 25 percent. (See fig. 20.) The majority of these services were categorized as
denials.
20
As discussed earlier, available IHS data on PRC program expenditures are limited to those facilities that are
federally operated, which in fiscal year 2017 represented about 46 percent of all IHS expenditures. The remaining
facilities were tribally operated and are not required to report these data to IHS.
21
According to IHS, IHS users living in rural areas often have to travel long distances for referral services.
22
IHS policy requires that deferred services be for elective care, rather than emergent or urgent care. Programs may
not defer payment for services already rendered, only for services that have not been received.
Page 20 GAO-19-74R Indian Health Service
Figure 20: Number of Denied and Deferred Purchased/Referred Care (PRC) Program Services (Federal and
Tribal), Fiscal Years 2013-2017
Note: Data represent PRC program requests from federally operated facilities—which in fiscal year 2017 represented about 46
percent of all IHS expenditures—and some tribally operated facilities, which are encouraged, but not required to report such data.
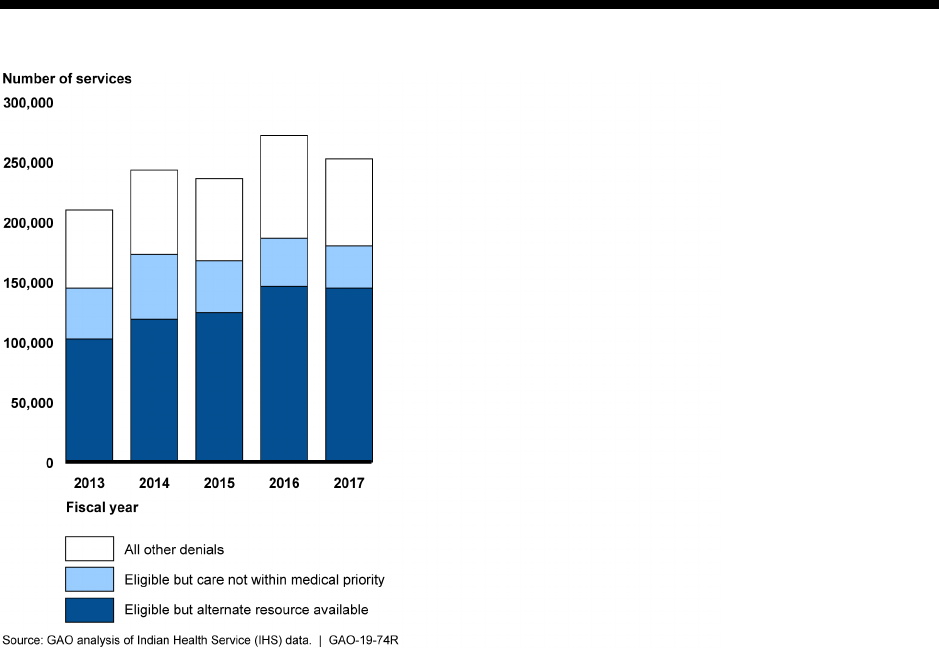
Federally and tribally operated facilities reported a variety of reasons for why services under the
PRC program were denied. The most common reason for the denial from fiscal years 2013
through 2017 was that the user had an alternate source of coverage for the service—such as
Medicaid or private insurance—to pay for the service, increasing from 102,409 denied requests
in fiscal year 2013 to 144,655 denied requests in fiscal year 2017. (See fig. 21.) The second
most common reason for denial under the PRC program was that the user’s needed health care
services were not within the medical priorities for which the facility had funding, although the
user was otherwise eligible.
23
Specifically, that reason accounted for 42,293 denials in fiscal
year 2013 and decreased to 34,988 denials in fiscal year 2017.
Those denied services included,
among others, inpatient services, outpatient services, and transportation services.
23
We found that facilities have often been limited to paying for only those services within the first category of the
medical priority system—emergency services to prevent the immediate death or serious impairment of the health of
the individual. See GAO-12-446. However, some facilities are able to pay for additional types of services.
Page 21 GAO-19-74R Indian Health Service
Figure 21: Number of Denied Purchased/Referred Care (PRC) Program Services (Federal and Tribal) by
Reason, Fiscal Years 2013-2017
Note: “All other denials” includes reasons such as emergency notification not provided within 72 hours and the patient residing
outside the PRC service delivery area, among others. Data represent PRC program requests from federally operated facilities—
which in fiscal year 2017 represented about 46 percent of all IHS expenditures—and some tribally operated facilities, which are
encouraged, but not required to report such data.
(102489)

This is a work of the U.S. government and is not subject to copyright protection in the United States.
The published product may be reproduced and distributed in its entirety without further permission
from GAO. However, because this work may contain copyrighted images or other material,
permission from the copyright holder may be necessary if you wish to reproduce this material
separately.
The Government Accountability Office, the audit, evaluation, and investigative
arm of Congress, exists to support Congress in meeting its constitutional
responsibilities and to help improve the performance and accountability of the
federal government for the American people. GAO examines the use of public
funds; evaluates federal programs and policies; and provides analyses,
recommendations, and other assistance to help Congress make informed
oversight, policy, and funding decisions. GAO’s commitment to good government
is reflected in its core values of accountability, integrity, and reliability.
The fastest and easiest way to obtain copies of GAO documents at no cost is
through GAO’s website (https://www.gao.gov). Each weekday afternoon, GAO
posts on its website newly released reports, testimony, and correspondence. To
have GAO e-mail you a list of newly posted products, go to https://www.gao.gov
and select “E-mail Updates.”
The price of each GAO publication reflects GAO’s actual cost of production and
distribution and depends on the number of pages in the publication and whether
the publication is printed in color or black and white. Pricing and ordering
information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077, or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard,
Visa, check, or money order. Call for additional information.
Connect with GAO on Facebook, Flickr, Twitter, and YouTube.
Subscribe to our RSS Feeds or E-mail Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
Contact:
Website: https://www.gao.gov/fraudnet/fraudnet.htm
Automated answering system: (800) 424-5454 or (202) 512-7470
Orice Williams Brown, Managing Director, WilliamsO@gao.gov, (202) 512-4400,
U.S. Government Accountability Office, 441 G Street NW, Room 7125,
Washington, DC 20548
Chuck Young, Managing Director, young[email protected], (202) 512-4800
U.S. Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
James-Christian Blockwood, Managing Director, spel@gao.gov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814,
Washington, DC 20548
GAO’s Mission
Obtaining Copies of
GAO Reports and
Testimony
Order by Phone
Connect with GAO
To Report Fraud,
Waste, and Abuse in
Federal Programs
Congressional
Relations
Public Affairs
Strategic Planning and
External Liaison
Please Print on Recycled Paper.
